Unmet medical needs in NAFLD and NASH
NAFLD (non-alcoholic fatty liver disease) comprises a spectrum of conditions starting with adiposity of the liver (fatty liver, steatosis hepatis) and ranging up to NASH (non-alcoholic steatohepatitis). Currently about 30% of the general population and 60-80% of people with type 2 diabetes are considered to be affected by NAFLD [1].
Premature mortality from NAFLD comes from the development of diabetes and cardiovascular disease and progression of the fatty liver to the more irreversible and aggressive NASH which again predisposes for incident liver cirrhosis and hepatocellular carcinoma [2]. Despite the potentially disastrous outcome of NAFLD and an increasingly rich knowledge concerning the underlying molecular pathogenesis no rational drugs and therapies specifically dedicated to the treatment of NAFLD are available yet.
In this blog we first provide a brief overview on the key pathogenetic drivers in NAFLD. Then we highlight the inherent opportunities and challenges for developers of lifestyle interventions and drugs tackling NAFLD. And last but not least we discuss some key issues related to the design and implementation of clinical trials in NAFLD and NASH.
If you want to learn more on Profil’s general perception of the liver’s role in health and disease you are invited to read our „Liver first? The liver in diabetes and cardiovascular disease“ series of blogs (part I, part II, part III).
Molecular traits in NASH and NAFLD: targets for lifestyle interventions and drugs
The pathogenetic mechanisms underlying the progression of NAFLD are complex but provide a plethora of potential targets for drug developers. According to a seminal concept presented by Christopher P. Day and Oliver F.W. James in 1998 [3], the progression of NAFLD is characterized by two hits, i.e. adiposis of the liver (first hit) and liver inflammation (second hit).
The Nobel laureates Michael Brown and Joseph Goldstein in 2008 explored the conception of a selective vs. a total insulin resistance of the liver when considering the metabolic derangements leading to vascular complications in NAFLD and type 2 diabetes. They explained why a selective insulin resistance more than a total insulin resistance of the liver adds to the pathogenetic devastation often seen in the course of NAFLD and type 2 diabetes [4].
We see a gap between the rich scientific knowledge on the pathogenetic traits underlying NAFLD/NASH and its translation into innovative lifestyle interventions and drugs available for an effective treatment of this disease.
NAFLD: the first hit
In NAFLD the first hit is a non-alcoholic fatty liver characterized by a potentially benign and reversible hepatocellular deposition of triglycerides. Insulin resistance of both liver and adipose tissue and a compensatory hyperinsulinemia play a key role in fatty liver development [5]. Impaired suppression of the hormone-sensitive lipase activity by insulin in the insulin resistant adipose tissue accounts for an increased flux of free fatty acids to the liver. In the liver the free fatty acids can be used for energy production via mitochondrial oxidation or for the synthesis of triglycerides. Triglycerides become either immediately stored in the liver or incorporated into very low-density lipoprotein particles released by the liver into the circulation.
In addition to an increased free fatty acid flux from the adipose tissue to the liver there is an increase in hepatic lipogenesis by forced expression of the sterol regulatory binding protein (SREBP)-1c stimulated by hyperinsulinemia which contributes to hepatic triglyceride accumulation. SREBP-1c is a transcription factor feeding into an orchestrated transcriptional activation of lipogenic genes. At the same time hyperglycemia activates the carbohydrate response element binding protein (ChREBP) which activates the expression of liver-type pyruvate kinase. This enzyme catalyses the conversion of phosphoenol pyruvate into pyruvate (glycolysis) which again enters the citrate cycle leading to the provision of additional acetyl-CoA for the synthesis of free fatty acids. ChREBP like SREBP-1c activates the transcription of lipogenic genes.
In the setting of insulin resistance the intermediary product malonyl-CoA inhibitis the carnitine palmitoyl transferase 1-catalysed free fatty acid entry into the mitochondria, thereby further shifting the free fatty acids metabolism from mitochondrial fatty acid oxidation towards the synthesis of triglycerides.
NAFLD: the second hit
Liver fat accumulation increases the hepatic susceptibility for a second hit. The second hit comprises a composite of free fatty acids, toxic lipids, reactive oxygen species as well as inflammatory cytokines and chemokines which promote liver injury and hepatocyte death. Cellular content such as DNA and damage-associated molecular patterns as well as reactive oxygen species produced by dying hepatocytes stimulate the Kupffer cells to release proinflammatory (like TNF-alpha, IL-1beta, IL-6) and profibrogenic (like TGF-beta) factors. Also chemokines (like CCL2) and gut-derived pathogen-associated molecular patterns contribute to mounting the second hit.
In chronic liver injury second hit generation appears to be self-perpetuating: reactive oxygen species enable the formation of aldehydes such as trans-4-hydroxy-2-nonenal and malondialdehyde. These diffusing toxines affect wider areas of liver tissue. Depletion of ATP, NAD and glutathione as well as increased levels of dysfunctional biopolymers may further aggravate the propagation of liver inflammation and hepatocyte death [5,6].
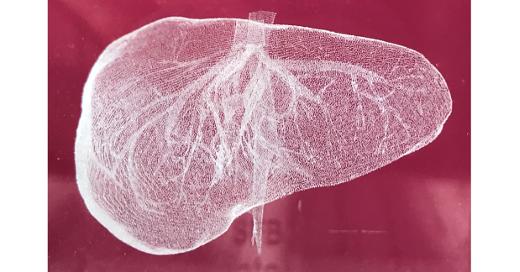
Hepatic stellate cells (HSCs) play a key role in transforming the second hit into liver fibrosis, liver cirrhosis, and finally liver failure [7]. Following liver injury HSCs undergo activation, thereby changing from a quiescent vitamin A-rich phenotype to proliferating, contractile, movable, and fibrogenic myofibroblasts. Activated HSCs imbalance extracellular matrix synthesis and degradation. That way they contribute to qualitative and quantitative changes in extracellular matrix composition and deposition. Although HSC activation and the remodelling of liver tissue are part of a wound healing response chronic liver injury as prevalent in NAFLD/NASH may increase the persistence of HSC activation leading to a progressive replacement of functional liver parenchyma with scar tissue, impaired vascular architecture and blood flow, and eventually liver failure [8,9,10].
Selective insulin resistance in NAFLD and cardiovascular disease
Key insights about the potential contribution of selective hepatic insulin resistance to the progression of NAFLD came from the seminal investigations on the liver-specific insulin receptor knockout (LIRKO) mice [11].
In these animals the insulin-receptor-dependent insulin signalling is specifically absent in the liver parenchymal cells. Although LIRKO mice display a severe resistance of hepatic glucose production towards insulin-induced suppression the animals don´t develop type 2 diabetes. They display beta-cell hyperplasia and a decreased hepatic insulin clearence which apparently compensate for the insulin resistance. However, when fed a pro-atherogenic diet LIRKO mice produced a significant dyslipidemia. Accordingly LIRKO mice on a pro-atherogenic diet showed a significantly increased incidence of atherosclerotic plaques [12].
Lessions from the LIRKO mice contributed to the conception of selective vs. total insulin resistance in NAFLD and type 2 diabetes. As outlined by Brown and Goldstein [13] under "healthy" conditions insulin suppresses hepatic glucose production (via phosphorylation and thereby inactivation of the transcription factor FoxO1). At the same time insulin stimulates the synthesis of free fatty acids and triglycerides (via activation of the transcription factor SREBP-1c), resulting in the maintenance of normoglycemia and adequate levels of triglycerides.
In the LIRKO mice total insulin resistance of the liver blocks both the insulin-induced suppression of hepatic glucose production and the insulin-induced stimulation of free fatty acid and triglyceride synthesis. This eventually accounts for the occurrence of hyperglycemia in the absence of hypertriglyceridemia. Hyperglycemia without hypertriglyceridemia probably has less severe consequences on the health of mice as compared to the combined hyperglycemia and hypertriglyceridemia established in LIRKO mice by feeding a pro-atherogenic diet.
From LIRKO it became clear that rather than hyperglycemia per se a selective insulin resistance of glucose production paired with unrestrained free fatty acid and triglyceride synthesis could mount a major contribution of the liver to the progression of NAFLD towards of type 2 diabetes and cardiovascular disease.
Combined hyperglycemia and hypertriglyceridemia is a prevailing finding also in human type 2 diabetes which can be explained by a selective insulin resistance of the human liver. While hyperinsulinemia fails to suppress the FoxO1-dependend hepatic glucose production it over-stimulates the SREBP-1-dependent synthesis of free fatty acids and triglycerides. The ticking pathogenetic time bomb of combined hyperglycemia and hypertriglyceridemia is planted which aggravates to fatty liver, weight gain, and overall disease progression.
As presented in the Edwin Bierman Award Lecture at the American Diabetes Association’s 75th Scientific Sessions [14] the conception of selective insulin resistance as a contributor to the development of cardiovascular disease has been extended to the vasculature. In vascular cells elevated levels of glucose, free fatty acids, and inflammatory cytokines as prevalent in progressive NAFLD selectively inhibit insulin’s anti-atherogenic actions mormally mediated via the IRS/PI3K/Akt pathway. At the same time pro-atherogenic insulin actions mediated by MAP-kinase pathways remain active.
Overall the data point to the need for a more differentiated view on insulin resistance with regard to affected target tissues, cell types, as well as metabolic, mitogenic and cytoprotective pathways.
A fatty liver can turn into a metabolic barrel burst
Although the fatty liver is considered the potentially non-progressive subtype of NAFLD its presence has been suggested to increase the risk of developing type 2 diabetes and cardiovascular disease.
Stefan et al. [15] have stratified obese people with a body mass index equal to or exeeding 30 kg·m-2 into an insulin sensitive and an insulin resistant group by using oral glucose tolerance test- and homeostasis model-derived indexes. They found that it is the fatty liver as well as an increased intima media thickness of the common carotid athery (an early marker of atherosclerosis) which distinguish the insulin sensitive obese (i.e the „metabolically healthy“) from the insulin resistant obese (i.e. those „at risk“ of diabetes and comorbid conditions).
Klöting et al. [16] stratified non-diabetic obese people having a body mass index between 42 and 48 kg·m-2 into an insulin sensitive and an insulin resistant group by measuring glucose infusion rates during a hyperinsulinemic euglycemic clamp experiment. The insulin resistant subgroup was characterised by a considerably higher amout of liver fat as compared to the insulin sensitive group.
Also the RISC (relationship between insulin sensitivity and cardiovascular disease) study population was analysed for a contribution of a fatty liver to the evolution of type 2 diabetes and cardiovascular disease. The RISC study was a large prospective observational cohort study of healthy people recruited by 19 trial centers in 14 European countries [17]. Insulin sensitivity was measured by using a hyperinsulinemic euglycemic clamp. A fatty liver index was used as a validated and non-invasive surrogate for the presence of a fatty liver in an otherwise healthy trial population. High fatty liver index values were associated not only with insulin resistance and a loss of glycemic control but also with increased intima media thickness, Framingtham risk scores for cardiovascular disease, liver enzymes, low-density lipoprotein cholesterol and systolic blood pressure, and with a decrease of high-density lipoprotein cholesterol and adiponectin [18].
When stratifying the RISC population for the presence of early carotid plaques it was observed that people with an increased fatty liver index were at an increased probability for athersclerotic lesions. When looking into the parameters used for fatty liver index calculation the plasma concentrations of gamma glutamyl transferase (GGT) emerged as an independent predictor of early carotid atherosclerosis [19].
Indeed, liver-derived GGT may be immediately involved in the aggravation of atheroscleorosis. GGT enzymatic activity has has been detected within sections of coronary atheroma from endoarteriectomy in vivo and suggested to promote a cysteinyl-glycine-triggered and iron-dependent redox cycling culminating in the formation of reactive oxygen species, oxidation of low-density lipoprotein, protease/anti-protease inbalances and smooth muscle cell proliferation, finally promoting plaque evolution and rapture [20]. 20-year longitudinal results from the Framingham offspring study indicate a prognostic value of GGT for the metabolic syndrom, cardiovascular diseases, and all-cause mortality [21]. Therefore elevated GGT is a candidate link between the presence of a fatty liver and the development of cardiovascular disease.
Also bidirectional interactions between insulin-resistant, inflamed adipose tissue and the diseased liver as mediated by the release of adipose-derived hormones, inflammatory cyto- and chemokines, free fatty acids, and hepatokines (e.g. FGF21, fetuin-A, IGF and IGFBPs, selenoprotein P, SHBG) have been recognized as pathogenetic drivers in the progression of NAFLD. Pro-inflammatory and pro-atherogenic mediators produced in the adipose tissue and the liver create a systemic state promoting peripheral insulin resistance, diabetes, and atherogenesis [22,23].
Most recently genome-wide and abdominal magnetic resonance imaging (MRI) data provided evidence that a genetically determined favorable adiposity phenotype is characterized by lower ectopic liver fat and lower risk of type 2 diabetes, heart disease, and hypertension [24]. This study further strengthens the consideration that the accumulation of liver fat makes the difference between the metabolically healthy but obese and the metabolically unhealthy obese people who are at higher risk for disease aggravation.
Medical need for personalized lifestyle interventions
Lifestyle changes have been recognised to be a cornerstone in the prevention of diabetes, NAFLD, NASH and cardiovascular disease [25]. As demonstrated recently by the DiRECT (diabetes remission clinical trial) investigators the sustainable remission of human type 2 diabetes caused by a tough dietary intervention (caloric restriction) was dependent on a decrease of liver and pancreas fat content [26]. This trial outcome added evidence to the twin cycle hypothesis published by Roy Taylor in 2008 [27,28]. In this framework a fatty liver-related dyslipidemia accounts for a fatty degeneration of the pancreas which again promotes beta-cell failure. This consideration immediately links the fatty liver to the loss of beta cell function leading to the precipitation of type 2 diabetes. Here the caloric restriction-induced decrease of pancreas and liver fat is considered the „reverse route from cure to cause“. Whether the success of caloric restriction in promoting the remission of type 2 diabetes should encourage pharmaceutical companies to advance the development of caloric restriction mimetics is not the question here.
In real-world there are multiple barriers to sustainable lifestyle interventions. Sustainably effective dietary regimes are difficult to implement and often hamper from a limited compliance of targeted people. There is a general gap between the broad availability of quality information on the impact of lifestyle changes for health promotion and chronic disease prevention on the one hand, and the translation of this knowledge into behavioural change on the other.
In addition the overweight and obese population is quite heterogeneous with regard to both, disease risk and susceptibility to specific lifestyle interventions. Therefore the usual lifestyle interventions may be too unfocused as a specific adjustment to individual risk patterns and personal capabilities is missing. Advanced individual risk assessment tools should enable a more accurate differentiation between metabolically healthy obese and obese at-risk, as well as the identification of healthy lean and lean but metabolically obese people.
Medium-term advancements in sensor development and non- or minimally invasive continuous metabolic monitoring combined with the exploration of digital biomarkers and individual „omics“ signatures may help to tailor lifestyle interventions to the individual needs and capabilities. People’s benchmarking with peer groups facilitated by the wide use of social media may strengthen self-motivation and thereby also promote adherence.
Overall we see the need for a holistic approach to lifestyle interventions, integrating technologically advanced and validated tools for risk assessment and metabolic profiling with a personally tailored implementation and follow-up of lifestyle interventions.
Medical need for rational pharmacotherapies
Until today no drug has obtained marketing approval specifically for the treatment of NAFLD or NASH. Current pharmacological treatments of NAFLD aim at managing cardiovascular risk factors including obesity, dyslipidemia, liver fat, hypertension and type 2 diabetes. Many established anti-diabetic drugs are currently under clinical investigation for their potential effectiveness in treating NAFLD and preventing the transition of a fatty liver towards NASH. Such drugs include metformin, dipeptidyl peptidase-4 (DPP-4) inhibitors, GLP-1 receptor agonists, SGLT-2 inhibitors, and thiazolidinediones [29].
From the recent pathogenetic insights it can be concluded that the improvement of hepatic insulin sensitivity should be one of the key objectives in NAFLD treatment. For drug developers this means that the design of insulin sensitizers should refer to a full understanding of the tissue and pathway specificity of insulin resistance. Potentially counterproductive health effects of non-specific insulin sensitizers should not be overlooked.
Particularly in the elderly a slight insulin resistance may reflect an adaptive response protecting the ageing cells from the deleterious action of dysfunctional protein accumulation [30]. Even more provocatively a cardio-protective role rather than the promotion of vascular disease has been attributed to the insulin resistance of specific signal transduction pathways [31,32]. Overall different semantics of insulin resistance should be addressed by the development and clinical evaluation of drugs for the treatment of NAFLD and NASH.
The development of antifibrotic therapies is a current focus in experimental and translational hepatology. Today the identification of therapeutic targetes very much focuses the hepatic dynamics in fibrogenesis and fibrolysis, i.e. the de novo formation and the removal of extracellular matrix and connective tissue [33]. There is a high diversity of fibrogenic and fibrolytic pathways whose activation depends on the pathogenic trigger and its primary target cells [34]. Antifibrotic target corridors for drug developers include the immune response, the regulation of platelet and endothelium function, and the extracellular matrix. Increased effectiveness is expected from the development of combination therapies interfering with different fibrogenic and/or fibrolytic pathways such as inflammation and extracellular matrix deposition, as well as from the consideration of the specific disease ethiology. In the condition of liver fibrosis caused by NASH amelioration of the second hit could be one key towards therapeutic effectiveness. Here molecules involved in insulin resistance and hyperglycemia, lipotoxic hepatocyte death and intestinal dysbiosis provide rational targets for both anti-inflammatory and antifibrotic effectiveness [35].
To which extent even advanced liver cirrhosis could still be reversible is a current matter of discussion, as is also the model systems to be used for a non- and preclinical characterisation of drug candidates [36]. Here the goal is to increase efficiency in translating preclinical success stories into human safety, tolerability and antifibrotic effectiveness.
Clinical trials in NAFLD/NASH
The design of clinical trials in NAFLD depends on the expected action mode of the drug candidate under investigation. NAFLD trials could focus on fatty liver (first hit) resolution mainly aiming at reducing liver fat and NASH progression. New drugs should specifically prevent mounting the second hit and/or reduce the hepatic susceptibility to the second hit which should be reflected in the clinical trial design and the definition of corresponding endpoints.
Alternatively NAFLD trials could focus on the resolution of existing liver fibrosis or even cirrhosis aiming at the regeneration of functional liver tissue. Also here the interception of the second hit must be addressed by including appropriate clinical trial endpoints. Only drugs that interrupt the self-perpetuating mechanisms feeding into liver fibrosis and cirrhosis will be effective in a sustainable treatment of NASH.
Proof-of concept (phase I/IIa) trials with a focus on fatty liver resolution should be designed to assess a potential reduction in liver fat (primary endpoint) by magnetic resonance imaging (MRI)- or magnetic resonance spectroscopy (MRS). Emerging data support the use of magnetic resonance imaging-derived proton density fat fraction (MRI-PDFF) as a non-invasive, quantitative, and accurate measure of liver fat content to assess the treatment response in early phase NAFLD trials [37].
In order to capture a more comprehensive activity profile and to widen the base for decision making on further development of a drug candidate it is recommended to also monitor changes in insulin sensitivity of the liver and adipose tissue by using 2-step hyperinsulinemic euglycemic clamp [38] combined with the infusion of stable isotope-labeled glucose and glycerol [39]. Also the re-distribution of body fat (MRI/MRS-based imaging), changes in body composition as accessible via air displacement plethysmography [40], and cardiovascular risk factors (e.g. assessment of the intima media thickness [41] and flow-mediated dilatation by means of high-resolution vascular ultrasound [42], telemetric ECG and 24-hour blood pressure monitoring [43], lipid profiling) deserve consideration.
Depending on the non- and pre-clinical data set it could be meaningful to address hepatic ATP synthesis (MRS) [44], energy expenditure (indirect calorimetry for assessment of resting energy expenditure and diet-induced thermogenesis, spiroergometry for the assessment of activity-induced energy expenditure, doubly labeled water method for the assessment of total energy expenditure) [45], as well as adipose tissue inflammation and metabolic activity (histological and gene expression analyses in adipose tissue biopsies) [46].
To economise trial conduct participants should be pre-selected by an abdominal ultrasound investigation [47] or by using surrogates for the presence of a fatty liver like the fatty liver index or signs of the metabolic syndrome [48] before performing more cost-intensive MRI/MRS-based investigations [49]. In case the candidate drug is expected to improve early stages of NASH e.g. by ameliorating liver inflammation, preventing progression of liver fibrosis or even reversing liver fibrosis, a pre-selection of trial participants for the presence of NASH by using non-invasive methods is recommended before sampling a liver biopsy for confirmation. Ultrasound transient elastrography (Fibroscan®) with controlled attenuation parameter [50] would be appropriate for simultaneously addressing fatty liver and liver fibrosis in patients with NAFLD [51]. Magnetic resonance elastography (MRE) is a novel method for the non-invasive assessment of liver fibrosis which needs to be further investigated for its use in NAFLD clinical trials [52]. A combination of elastrographic assessments with a panel of serum markers for hepatocyte apoptosis (e.g. cytokeratin-18 alone or combined with FGF-21) and/or liver fibrosis (e.g. SteatoTest) and/or with calculation of the NAFLD fibrosis score could increase the accuracy of NASH detection [53]. It is worthy of note that limitations on the use of liver biopsies related to invasiveness of sampling, high sampling variability, and not indicating early changes in fibrogenic and fibrolytic activity, are increasingly made a subject of debate.
Although liver fibrosis has multiple etiologies NASH is considered to be the dominant disease indication for the development of antifibrotic drugs [54]. Valuable insight about the human potential for fibrosis regression comes from the treatment of viral hepatitis. In patients with chronic hepatitis B a long-term antiviral treatment resulted in a reversal of liver fibrosis and cirrhosis with remarkable reductions in inflammation and necrosis after 1 year and improvements in fibrosis and even cirrhosis after approximately 5 years [55]. In morbididly obese patients with NASH bariatric surgery led to a clinically relevant reduction in the NASH activity score after 1 year. The antifibrotic effect of bariatric surgery was less pronounced during this observation interval [56], suggesting the requirement for a longer-term follow-up in order to capture a continued fibrosis regression. For the design of antifibrotic drug trials this implies that a significant improvement in necro-inflammation often occurs after 1 year. Longer drug exposure is needed to establish antifibrotic effectiveness at the level of histologic classification.
The American Association for the Study of Liver Diseases (AASLD) recently sponsored an emerging trends conference on strategies and endpoints of antifibrotic drug trials [57]. Regulatory authorities require demonstration of impact at the level of hard clinical endpoints which in anti-fibrotic drug trials would be the prevention of liver cirrhosis with their inherent risk of decompensation, hepatocellular carcinoma, or death. Optionally, the use of surrogate endpoints can be considered provided they are reasonably likely to reflect clinically relevant outcomes.
Conclusion
Individual pathogenetic traits underlying NAFLD and its progression towards diabetes and cardiovascular disease, NASH, liver cirrhosis and hepatocellular carcinoma are increasingly well understood. This is an essential requirement for tackling the challenge posed by NAFLD in general and NASH in particular by the provision of personalized lifestyle interventions and drugs.
In the clinical development of drugs targeting NAFLD the clinical trial population needs to be carefully defined in order to avoid meaningless trial outcomes. Non-invasive technologies for the assessment of liver fat and liver stiffness should be combined with sophisticated metabolic assessments using clamp methodology in combination with stable isotope-labeled tracer compounds and the assessments of biomarkers. The goal is to early capture the full pharmacodynamic potential of the drug candidate under clinical development. The increased susceptibility of the fatty liver to agents which are potentially hepatotoxic (second hit) requires special attention when establishing the safety and tolerability profile of drug candidates.
In NAFLD the prescription of drugs should be preceded by lifestyle interventions such as caloric restriction which has been proven to reduce liver fat and to reverse the pathogenesis of diabetes up to the remission of the disease in a considerable sub-group of patients [58]. To achieve a wider sustainability of lifestyle interventions we need technologically advanced tools for risk assessment and metabolic profiling in order to inform the personalization of lifestyle interventions and make the sustainability of them a reality.
Overall tackling NAFLD and NASH is not about picking low hanging fruits. A multifaceted and collaborative approach to early diagnostics, interception, prevention, and treatment is needed to make the common fight against this disease complex successful.
If you are interested we also invite you to watch our free online seminars NASH and Diagnosis of NAFLD.




