Despite treatments becoming more effective and despite more adequate control of the risk factors (e.g. smoking, inadequate glycemic control or hypertension), patients with diabetes continue having increased risk of chronic kidney disease (CKD) (1). It is estimated that diabetic nephropathy affects approximately 30% of subjects with diabetes, who could eventually develop end-stage renal disease (2) resulting in a significant negative impact on life quality and life expectancy.
The sodium/glucose cotransporter 2 (SGLT2) inhibitors have been intensively investigated in the previous years due to their mechanism of action involving renal excretion of glucose. Large studies have shown the potential of these drugs to improve glycemic control and also to improve cardiovascular (CV) outcomes (3, 4). The EMPA-REG OUTCOME trial (3) and the CANVAS program (4) evaluated the efficacy of SGLT2 inhibitors in reducing the occurrence of CV endpoints. Both trials had secondary endpoints to evaluate the progression of nephropathy in the subjects studied.
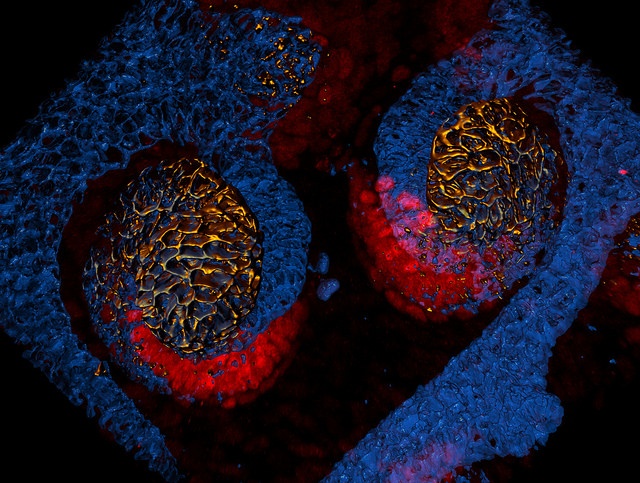
Credit: eLife/Lindstrom at al
The EMPA-REG OUTCOME trial
This study with empagliflozin included over 7000 patients with type 2 diabetes mellitus (T2DM), established CV disease and eGFR (estimated glomerular filtration rate) > 30 ml/min/1.73m2. The primary end-point was composite major adverse cardiac events (MACE) outcome (3). A secondary outcome was a composite microvascular outcome that included: initiation of retinal photocoagulation, vitreous haemorrhage, diabetes-related blindness or incident or worsening nephropathy (5).
Subjects in the empagliflozin group had 24% less primary outcome events (hazard ratio 0.86; 95% CI, 0.74 – 0.99). The results of the secondary endpoints showed a significant relative risk reduction of 38% in the microvascular outcome (hazard ratio 0.62; 95% CI, 0.54-0.70), which was driven mainly by the renal component (hazard ratio 0.61; 95% CI, 0.53-0.70).
Other renal outcomes in the EMPA-REG OUTCOME trial included incident or worsening nephropathy and incident albuminuria. Nephropathy was defined as progression to macroalbuminuria, doubling of the serum creatinine level, initiation of renal-replacement therapy, or death from renal disease. The results showed a significant relative risk reduction of 39% in incident or worsening nephropathy in subjects taking empagliflozin (hazard ratio 0.61; 95% CI, 0.55–0.69). There was no significant between-group difference in the rate of incident albuminuria (hazard ratio 0.95; 95% CI, 0.87–1.04).
An interesting observation in this study was the behaviour of the eGRF curves over time, which showed an initial decrease at the beginning of the treatment with empagliflozin; this initial drop was reversed once the medication was stopped and returned to levels close to the initial eGFR. The subjects on placebo showed the usual progressive deterioration of the eGFR, while the subjects on empagliflozin seemed to have a slower progression.
The CANVAS Program
The CANVAS program included two trials (CANVAS and CANVAS-R), and focused on canagliflozin and cardiovascular endpoints. Over 10000 subjects with T2DM at high CV risk and eGFR > 30 ml/min/1.73m2 were included in both trials (4). The primary endpoint was a composite MACE outcome. One of the secondary endpoints was progression of albuminuria, defined as 30% increase, change from normoalbuminuria to micro or macroalbuminuria or change from microalbuminuria to macroalbuminuria. Additionally, the trial included some exploratory renal outcomes:
- Regression of albuminuria
- A renal composite comprising a 40% reduction in eGFR sustained for at least two consecutive measures, the need for dialysis or transplantation, or death from renal causes.
Subjects in the canagliflozin group had 24% less primary outcome events (hazard ratio 0.86; 95% CI, 0.75 to 0.97). Progression of albuminuria occurred less frequently in the canagliflozin group (hazard ratio 0.73; 95% CI, 0.67 to 0.79). Regression of albuminuria also occurred more frequently in the canagliflozin group (hazard ratio 1.70; 95% CI, 1.51 to 1.91). The composite outcome (40% reduction in eGFR, renal-replacement therapy, or renal death) occurred less frequently in the canagliflozin group (hazard ratio of 0.60; 95% CI, 0.47 to 0.77).
Significance of the evidence
The results reported above suggest that SGLT2 inhibitors might improve renal outcomes and slow progression of kidney disease. However, care should be taken when making assumptions, primarily because the follow up time in both the EMPA-REG OUTCOME trial and the CANVAS program does not allow any conclusion regarding the long-term effect of SGLT2 inhibitors on kidney function. Although other renal endpoints were investigated in the studies, their occurrence was very low, and this does not allow for definitive conclusions.
Regarding the positive findings of albuminuria it should be mentioned, that it is not considered a good marker of renal function improvement, mostly because it might be linked to the decrease in GFR. Additionally, the benefits in GFR observed in the EMPA-REG OUTCOME trial still need to be confirmed for other SGLT-2 inhibitors.
Finally, the results are just applicable for a collective of patients with T2DM and established CV risk, which means that further investigations are needed to conclude that SGLT2 inhibitors tackle CV and renal mortality in the long term in subjects with less risk factors.
The issue of hyperfiltration
The pathophysiology of CKD is complex and many factors seem to contribute to its development and progression. One of the mechanisms that have been discussed as responsible for the damage of the glomerulus is hyperfiltration, which seems to be a compensatory phenomenon occurring as a response to nephron loss. Hyperfiltration would, in the long-term, damage the nephron and contribute to progression of CKD.
In diabetes there is increased reabsorption of glucose in the proximal tubule, accompanied by increased sodium cotransport. This leads to decreased solute load in the macula densa and to a consequent deactivation of the tubuluglomerular feedback. As a result there are increased GFR and hyperfiltration (6).
There is evidence that SGLT2 inhibitors reduce renal hyperfiltration, probably by affecting tubular-glomerular feedback mechanisms (7). Reduction of hyperfiltration would be responsible for the initial drop in GFR observed at the beginning of treatment with SGLT2 inhibitors and to the retarded decline of renal function (6) observed when the medication is stopped.
Other factors
The entire cascade of effects caused by SGLT2 inhibition is still being investigated. One of the effects of these drugs is blood pressure reduction, mainly due to the reduction in extracellular fluid volume. As lowering blood pressure is already an effective measure for primary and secondary prevention of CKD it is, in principle, not surprising that this effect could also contribute to the improved renal outcomes observed. On the other hand, the effect of SGLT2 inhibition on blood pressure is rather small, and it is rather unlikely that this is the only explanation for the benefits observed.
Both high levels of uric acid and weight are factors affecting progression of CKD (2) and it is stablished that SGLT2 inhibitors reduce both. Nevertheless, whether these effects contribute to the preservation of the renal function remains unknown.
Conclusion
The class of SGLT2 inhibitors has great potential to improve glycemic control and to reduce cardiovascular mortality. There are encouraging results showing a slower decline in renal function in patients with diabetic nephropathy. There are still a number of open questions, in particular whether the observed effects would apply to patients without CVD. Further efforts such as the CREDENCE trial (Canagliflozin and Renal Endpoints in Diabetes with Established Nephropathy Clinical Evaluation) will be needed to discern the impact of SGLT2 inhibitors on renal outcomes in individuals with nephropathy in greater detail.
References
- Stanton RC. Sodium glucose transport 2 (SGLT2) inhibition decreases glomerular hyperfiltration: is there a role for SGLT2 inhibitors in diabetic kidney disease? Circulation. 2014;129(5):542-4.
- Fioretto P, Zambon A, Rossato M, Busetto L, Vettor R. SGLT2 Inhibitors and the Diabetic Kidney. Diabetes Care. 2016;39 Suppl 2:S165-71.
- Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373(22):2117-28.
- Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med. 2017;377(7):644-57.
- Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. N Engl J Med. 2016;375(4):323-34.
- Scheen AJ, Delanaye P. Effects of reducing blood pressure on renal outcomes in patients with type 2 diabetes: Focus on SGLT2 inhibitors and EMPA-REG OUTCOME. Diabetes & metabolism. 2017;43(2):99-109.
- Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129(5):587-97.




