Hepatoselective insulin analogues-a dream may become reality?
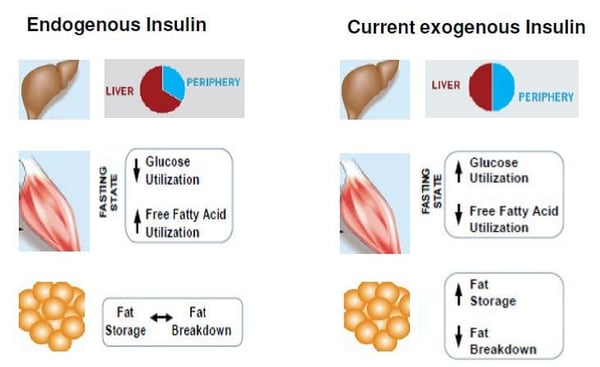
It has always been a dream to provide insulins for diabetes therapy mimicking endogenous insulin secretion and action. Normal physiology means that insulin is released into the liver through the portal vein from the pancreatic islets of Langerhans. Therefore, the liver is physiologically exposed to higher insulin concentrations than the periphery.
In most cases new insulin developments are focused on modifying patterns of insulin absorption from subcutaneous depot by altering the formulation or developing other methods of delivery. However, in addition to an improved absorption, distribution is an important contributor to insulin action. Distribution factors are mainly affected by accessibility to target tissue. While the peripheral capillary wall is lined by continuous epithelium, the transfer is restricted to small molecules. In contrast to this the high fenestrated epithelial cells lining the vascular sinusoids of the liver offer optimal accessibility for large-sized plasma protein molecules to the direct surface of hepatocytes (1).
To overcome the challenges of peripheral subcutaneous insulin delivery it is important to develop an insulin analogue exerting a direct and strong effect on the liver by using predominantly the barrier-free passage through the vascular sinusoids of the liver. Using this approach the novel hepato-preferential insulin has the potential to restore the physiological normal portal to peripheral insulin gradient. Furthermore, a hepatoselective insulin analogue should be characterized by a low-receptor binding affinity resulting in a reduced level of first-pass hepatic extraction and thereby controlling the degree to which the periphery is insulinized (2).
Source: Derived from Dimitriadis et al. Diabetes Res Clin Pract.2011;93(suppl):S52-S59
Loss of the normal hepatic to peripheral insulin gradient results in relative peripheral hyperinsulinaemia and under-insulinization of the liver (3) which leads to metabolic abnormalities like dyslipidaemia (inhibition of lipolysis in peripheral adipose tissue), glycemic fluctuations (caused among other by an increased glucose utilization and a reduced fatty acid utilization in muscle, accompanied by a suppressed glucagon secretion from pancreas), and a reduced hepatic IGF-1 production. Hepatic glucose production can also be suppressed by selective increment in peripheral insulin (4).
To reproduce the hepato-preferential effects of endogenously secreted insulin might reduce complications associated with current insulin therapy (5). Clinical short-term studies demonstrated advantages like weight benefit, lower rate of nocturnal hypoglycemia and the potential of decreased prandial insulin requirements particularly in patients with diabetes when compared with conventional basal insulin analogue therapy (6,7,8).
Our expertise offers a wide range of methodologies related to the evaluation of hepatoselective insulins. We are able to find an appropriate design for your approach including analysis and interpretation of the results. The hyperinsulinemic euglycemic clamp technique might be used for directly determining metabolic glucose disposal rate in humans. To assess endogenous glucose production including metabolic fluxes the clamp technique might be combined with an infusion of stable isotope labelled ([6.6]-2H2-glucose) deuterium glucose (natural abundance). Additional tracer techniques may be used simultaneously to explore the effects of these insulin analogues on liver fat and whole body lipid physiology. To measure directly adipose tissue lipolysis, the microdialysis technique might be performed. If you are interested in the evaluation of the deposition of triglyceride into adipose tissue, different biopsy techniques are available.
[1] Herring R, Jones R H, Russell-Jones L. Hepatoselectivity and the evolution of insulin. Diabetes, Obesity and Metabolism. 2014; 16: 1–8.
[2] Chan S, Steiner D. Insulin through the ages: phylogeny of a growth promoting and metabolic regulatory hormone. Am Zool 2000; 40: 213–222.
[3] Hordern SVM, Wright JE, Umpleby AM, Shojaee Moradie F, Amiss J, Russell-Jones DL. Comparison of the effects on glucose and lipid metabolism of equipotent doses of insulin detemir and NPH insulin with a 16-h euglycaemic clamp. Diabetologia 2005; 48: 420–426.
[4] Sindelar D K, Chu Ch A, Rohlie M, Neal D W, Swift L L , Cherrington A D. The role of fatty acids in mediating the effets on peripheral insulin on hepatic glucose production in the conscious dog. Diabetes 1997; 46:187-196.
[5] Moore M C, Smith M S, Sinha V P,2 Beals J M, Michael M D, Scott J. Jacober S J, and Cherrington A D. Novel PEGylated Basal Insulin LY2605541 Has a Preferential Hepatic Effect on Glucose Metabolism. Diabetes 2014;63:494-504.
[6] Rosenstock J, Bergenstal RM, Blevins TC, et al. Better glycemic control and weight loss with the novel long-acting basal insulin LY2605541 compared with insulin glargine in type 1 diabetes: a randomized, crossover study. Diabetes Care 2013;36:522–528
[7] Sinha VP, Howey DC, Choi SL, Mace KF, Heise T. Steady-state pharmacokinetics and glucodynamics of the novel, long-acting basal insulin LY2605541 dosed once-daily in patients with type 2 diabetes mellitus. Diabetes Obes Metab 2014;16:344–350.
[8] Heise T, Howey DC, Sinha VP, Choi SL, Mace KF. Steady-state pharmacokinetics (PK) and glucodynamics (GD) of the novel, long-acting basal insulin LY2605541 dosed once-daily (QD) in patients with type 2 diabetes mellitus (T2DM) (Conference Abstract). Diabetes 2012; 61(Suppl. 1): A256.




