The landmark trials DCCT/EDIC trials show how important good glycemic control is for the prevention of late complications in type 1 diabetes (T1D). According to the American Diabetes Association (ADA) an HbA1c target value of less than 7% should be targeted throughout all age groups to reduce the risk of late complications unless safety issues for individual patients or patients groups indicate higher HbA1c goals. However, most patients have difficulties to reach this target value despite improvements in diabetes therapy options during the last years. Especially the age group between 15 and 25 years have significantly higher HbA1c levels as analysis of data of various countries show [1]. The analysis of an US database, the so-called T1D Exchange registry which contains data of more than 35000 patients with T1D, indicate that glycemic control in adolescents and young adults seems to get even worse in the past years as from 2012 until 2018 the average HbA1c has increased, particularly in the younger age groups [2].
The causes of poor diabetes control in adolescents and young adults are many. In addition to the influence of hormones during puberty, which make achieving HbA1c targets more difficult, young adults face also new challenges such as leaving the parental home and deciding on a career, which presumably have a negative influence on the adherence to diabetes therapy recommendations [1]. But what can be done to improve diabetes management not only in this vulnerable patients but in all age groups?
Part of the solution might be the use of technology. CGM systems and insulin pumps are already widely used particularly for the treatment of young T1D patients. The benefit of such technologies, especially CGM was shown in many randomized studies and this positive influence is already observable also in the T1D Exchange registry population as recently reported by Miller et al [3]. The authors reported that pump users throughout all age groups had lower HbA1c levels compared to patients on MDI treatment. Moreover, the use of a CGM system was even more effective as it substantially lowered average HbA1c compared to non-CGM users and this positive effect was comparable if CGM was combined with an insulin pump or MDI therapy. This demonstrates that the knowledge about real time glucose levels is one of the most important factors that helps to improve diabetes control. However, the general shape of the HbA1c curve over all age groups has not changed so that adolescents and young adults still have the highest HbA1c levels compared to adults.
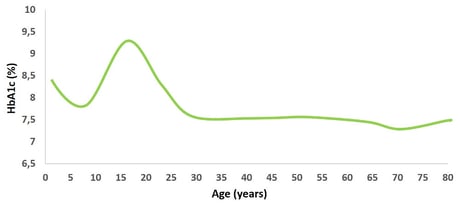
Figure: Graphical overview of HbA1c over lifetime similar to Miller et al [3].
According to Miller et al. also socioeconomic status (SES) has an important impact on glucose management. Patients with a lower income had substantially higher HbA1c level compared to patients with higher income throughout all age groups and this picture becomes even worse for people without any health insurance. The lower SES subgroup also benefited from CGM use as average HbA1c was lower in CGM user compared to non-CGM user but the general number of non-device users is substantially higher in the low SES than in the higher SES group. However, the authors also discussed that the T1D Exchange registry is not population based as only data from specialized diabetes clinics and not from general practitioners are included, so it is likely that the true average HbA1c in the US T1D population might be underestimated by this registry data.
For Germany, similar analyses have been done in the past, which also reported higher HbA1c levels during adolescence and lower values during adulthood. For such analyses, data from the German/Austrian Prospective Diabetes Follow-up Registry (DPV) was used that includes data from more than 400 diabetes specialists and diabetes clinics. The comparison of the US T1D Exchange registry with the German/Austrian DPV showed that HbA1c level were in general up to 1% higher in the US T1D Exchange registry compared to the DPV pediatric population [4]. Less than 20% of children in the age of 12 to <18 years of the US registry achieved an HbA1c below 7.5% while nearly 40% of children in DPV of the same age group reached this goal. Only in adulthood from an age of 30 years onwards, HbA1c levels were comparable between both registries. The underlying reasons for these substantial differences between the two registries are not completely clear but may be due to systemic differences regarding medical care, diabetes training, nutritional behavior and diabetes self-management as well as regulatory issues and general differences in health insurance coverage between both regions.
 Also in Germany an association between socioeconomic status and diabetes treatment and control could be observed. The group around Auzanneau et al. could show for patients living in German areas with a higher grade of deprivation that these have higher average HbA1c levels compared to patients living in least deprived areas [5]. The usage of diabetes technology such as insulin pumps or CGM systems and also of novel insulin formulations such as long-acting insulin analogues was also less widely used in the more deprived areas. These data show that despite a general cost coverage by the German health insurances not all T1D patients have equal access to diabetes technologies presumably resulting in less well controlled glucose control.
Also in Germany an association between socioeconomic status and diabetes treatment and control could be observed. The group around Auzanneau et al. could show for patients living in German areas with a higher grade of deprivation that these have higher average HbA1c levels compared to patients living in least deprived areas [5]. The usage of diabetes technology such as insulin pumps or CGM systems and also of novel insulin formulations such as long-acting insulin analogues was also less widely used in the more deprived areas. These data show that despite a general cost coverage by the German health insurances not all T1D patients have equal access to diabetes technologies presumably resulting in less well controlled glucose control.
The apparent link between diabetes technologies and lower HbA1c level across all age groups shows that the efforts of research and technology developments in recent decades are successful and can improve the overall care of type 1 diabetes patients. Nevertheless, much remains to be done to provide all diabetes patients with access to new diabetes technologies, but also to further improve diabetes control among young people. It remains to be seen to what extent further technical developments such as closed loop systems will enable T1D patients to reach the HbA1c target of less than 7%.




