Profil uses transient elastography with controlled attenuation parameter in order to pre-identify potential trial participants for the presence of liver fat and/or the presence of an intermediate state of liver fibrosis. Dependent on the outcome subsequently MR (magnetic resonance)-based methods and liver biopsy are available for further substantiating the findings. The great advantage of this non-invasive and quick approach is economising trial conduct by reducing the number of more elaborate examinations and controlling the sample size required for a meaningful trial design. This blog text describes the transient elastography method in the context of the increasing interest in treating subjects with NAFLD (non-alcoholic fatty liver disease).
NAFLD, a common disease with links to diabetes and cardiovascular disease
Recently the diagnosis of NAFLD and furthermore the development of a chronic liver disease is gaining more and more importance and consideration in the care of patients with type 2 diabetes. Details about the multifaceted relationship between NAFLD, diabetes, and cardiovascular disease have been discussed by Prof. Freimut Schliess in a blog post and in one of our online seminars.
According to most recent epidemiological studies, the prevalence of NAFLD is 25 % globally. There are several diseases that could occur in parallel to NAFLD, e.g. 70% of the NAFLD patients present with dyslipidaemia, 50% with adipositas and 22% with type 2 diabetes mellitus. NAFLD is the high-level term for the whole spectrum of fatty liver diseases not caused by excessive alcohol consumption. The potential development of liver cirrhosis as end-stage condition of NAFLD is shown in the figure below:
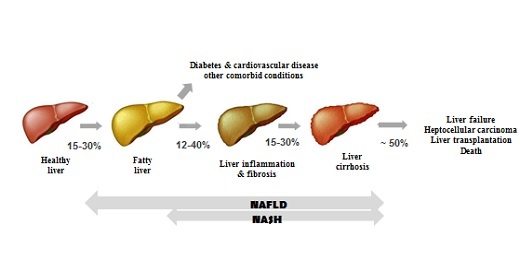 In case of developing NASH, it has been proven that this condition in addition to its potential to increase the cardiovascular disease risk can also lead to the development of a hepatocellular carcinoma (HCC).
In case of developing NASH, it has been proven that this condition in addition to its potential to increase the cardiovascular disease risk can also lead to the development of a hepatocellular carcinoma (HCC).
As stated in the AASLD guidelines, taking and analysing a liver biopsy is still considered the gold standard for securing a diagnosis of NAFLD. However, such an invasive method might cause complications such as bleeding, infections, etc. Also the limitations on the use of liver biopsies related to invasiveness of sampling, high sampling variability, and not indicating early changes in fibrogenic and fibrolytic activity are increasingly debated. Accordingly, there is ongoing research on the development of non-invasive methods such as specific serologic biomarkers indicating hepatocellular apoptosis (e.g. CK18, FGF21, etc.); indices as the Fatty Liver index (FLI) or the Hepatic Steatosis index.
Transient elastography
A non-invasive method called transient elastography has been developed that can measure liver stiffness (fibrosis) and fat proportion (steatosis) simultaneously on the same volume of tissue (3 cm²). The measurements are safe, reproducible and quantitative. For the measurement of steatosis a specific software option (CAP = Controlled Attenuation Parameter) is needed. The method is commercially available under the marketed name Fibroscan®. Below are details with regards to the liver stiffness and liver fat measurements performed with it:
Liver stiffness (Fibrosis)
- The stiffness is computed from the elastogram being a graphic representation of the shear wave propagation as a function of time and depth.
- The Young’s Modulus (E), also known as elastic modulus, is expressed in kiloPascal (kPa)
Liver fat proportion (Steatosis)
- The quantification of steatosis is performed via the CAP tool which is computed from the ultrasound acquired for stiffness measurement.
- The ultrasound attenuation corresponds to the decrease in amplitude of ultrasound waves as they propagate through the liver.
- CAP is expressed in decibel per meter (dB/m).
A comparison study of transient elastography with liver biopsy for the diagnosis of NAFLD and severity grading of liver fibrosis demonstrated high accuracy of transient elastography measurements. And although other studies have also identified potential confounders for results obtained with transient elastography, for example the association between liver stiffness and NAFLD seems less robust in patients with hepatitis C, the method is generally considered a viable alternative to the use of liver biopsy in the routine diagnostic assessment of NAFLD.




