HbA1c as gold standard marker of glycemic control
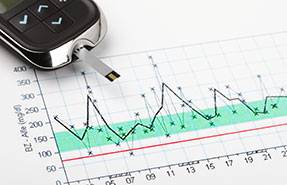
Hemoglobin (Hb) A1c results from the glycation of hemoglobin in erythrocytes and reflects the mean glycemic exposure over the past 2-3 months. Due to its high specificity and reproducibility, HbA1c is an important diagnostic tool and serves as a gold standard biomarker for glucose control, in particular because it has been established as a predictor of patient-oriented outcomes such as microvascular (and to a lesser extent macrovascular) diabetic complications in both patients with type 1 and type 2 diabetes. Although HbA1c is highly reliable, it does have some limitations. Postprandial excursions only make a minor contribution to overall HbA1c-levels, so that improvements in these short-lived glycemic peaks usually do not lead to pronounced changes in HbA1c. Moreover, interpretation of HbA1c-levels has been shown to be problematic in some populations [1], such as patients with anaemia or advanced nephropathy [2] [3]. This observation likely reflects shortened erythrocyte survival time resulting in less time for hemoglobin and glucose to chemically interact, so that HbA1c levels do not necessarily reflect mean blood glucose control under these conditions.
Alternative markers of glycemic control
Therefore, non-traditional glycemic markers like fructosamine, glycated albumin and 1,5-anhydroglucitol (1,5 AG) may be useful as alternatives or adjuncts to HbA1c as they provide important information on short-term (up to 2–4 weeks) glycemic control with a better reflection of glycemic fluctuations than HbA1c [4]. However, there are some differences between these biomarkers that need to be taken into account when choosing the optimum biomarker(s) for the assessment of glycemic control in clinical trials.
Fructosamine, a ketoamine resulting from glycation reactions between glucose and serum proteins (predominately albumin) is a marker of endogenous glucose exposure over a period of 2 to 3 weeks. It, therefore, is an easily measurable and relatively inexpensive marker of short-term diabetes control. However, its concentration is quite variable and affected by concentration changes of the various components (in particular proteins, e.g. in patients with nephrotic syndrome) and also by changes in bilirubin and uric acid. To reduce variability it has been suggested to standardise fructosamine to a serum albumin concentration of 40 g/l [5]. However, this approach has not become a universal standard.
Glycated albumin (GA) reflects the proportion of glycated albumin to total serum albumin and, therefore, offers certain advantages over fructosamine as it is not impacted by anaemia and changes in serum albumin levels [6]. However, GA tends to be lower in obese subjects with a high percentage of body fat mass [7]. It has been suggested as a marker for short-term glycemic control (the half-life of glycated albumin is 12-19 days), e.g., in gestational diabetes, and has been shown to be more reliable than HbA1c in patients undergoing hemodialysis [8]. Moreover, its glycation speed is ten times faster than that of HbA1c leading to a better correlation with postprandial hyperglycemia [9]. Several methods have been used to quantify GA but no uniform standard has been established yet. The costs for GA-determinations are considerably higher than those for fructosamine.
1,5-AG (a naturally occurring dietary polyol) is a marker of glycemia-induced glycosuria, since reabsorption of filtered 1,5-AG in the proximal tubule is competitively inhibited by glucose [10]. Lower serum 1,5-AG, therefore, reflects high circulating glucose with glycosuria in the past 24 hours providing a metric for time spent in hyperglycemia. Therefore, 1.5-AG is an indicator of high glycemic variability (i.e., pronounced within-day glycemic fluctuations) even if HbA1c or blood glucose measurements remain near-normal [11]. In patients with poor glycemic control, permanent glycosuria leads to low 1,5-AG concentrations that then reflect both fasting and postprandial glycemic deteriorations. As 1,5-AG mainly covers glycemic fluctuations over one treatment day, it is often necessary to do repeated measurements in clinical trials despite the fairly high costs of this assay. One major limitation of 1,5-AG is that it cannot be used in patients treated with SGLT-2 inhibitors as these agents cause glycosuria and, therefore, lead to low 1,5-AG concentrations even in well-controlled patients.
Summary
Overall, alternative markers of glycemic control, when used wisely, can provide important information instead of or in addition to HbA1c-measurements. It is important to understand, however, that none of these non-traditional markers have been validated for the prediction of microvascular or macrovascular complications.
For each particular trial and question to be answered, one should carefully assess which markers for glycemic control make most sense in the specific situation. There is no one-fits-all answer to this question. Profil Germany is experienced in the design of optimal studies and will be happy to assist you when making decisions like choosing markers for glycemic control or any other trial design related issues.
References
[1] Rubinow KB, Hirsch IB. Reexamining metrics for glucose control. JAMA 2011; 305:1132–1133.
[2] Freedman BI, Shenoy RN, Planer JA, et al. Comparison of glycated albumin and hemoglobin A1c concentrations in diabetic subjects on peritoneal and hemodialysis. Perit Dial Int 2010; 30:72–79.
[3] Peacock TP, Shihabi ZK, Bleyer AJ, et al. Comparison of glycated albumin and hemoglobin A(1c) levels in diabetic subjects on hemodialysis. Kidney Int 2008; 73: 1062–1068.
[4] Selvin E, Francis LM, Ballantyne CM, Hoogeveen RC, Coresh J, Brancati FL, Steffes MW. Nontraditional markers of glycemia: associations with microvascular conditions. Diabetes Care 2011; 34: 960 –7.
[5] Howey, JE; Browning, MC; Fraser, CG: Assay of serum fructosamine that minimizes standardization and matrix problems: use to assess components of biological variation: Cinical Chemistry 33: 269 1987
[6] Kim D, Kim KJ, Huh JH, Lee BW, Kang ES, Cha BS, et al. The ratio of glycated albumin to glycated haemoglobin correlates with insulin secretory function. Clin Endocrinol (Oxf) 2012;77:679-83.
[7] Lee JE. Alternative biomarkers for assessing glycemic control in diabetes: fructosamine, glycated albumin, and 1,5-anhydroglucitol. Ann Pediatr Endocrinol Metab 2015;20(2):74-8.
[8] Roohk HV, Zaidi AR. A Review of Glycated Albumin as an Intermediate Glycation Index for Controlling Diabetes. J Diabetes Sci Technol 2008; Vol 2, 6: 1114-1121.
[9] Hirsch IB, Brownlee M. Beyond hemoglobin A1c—need for additional markers of risk for diabetic microvascular complications. JAMA 2010;303:2291-2.
[10] Buse JB, Freeman JLR, Edelman SV, Jovanovic L, McGill JB. Serum 1,5-anhydroglucitol (GlycoMark): a short-term glycemic marker. Diabetes Technol Ther 2003;5:355–363.
[11] Stettler C, Stahl M, Allemann S, et al. Association of 1,5-anhydroglucitol and 2-h postprandial blood glucose in type 2 diabetic patients. Diabetes Care 2008;31: 1534–1535.




