Part A: Macrovascular Function
Diabetes mellitus is associated with numerous micro- and macrovascular complications. In patients with type 2 diabetes, macrovascular complications like stroke or myocardial infarction are the leading cause of an increased morbidity and mortality. Hyperglycaemia and insulin resistance are considered to represent the two main pathologic components in the development and progression of vascular disease in patients with type 2 diabetes mellitus.
Diabetes related vascular impairment can be detected even in a preclinical stage by the use of several biomarkers.
Endothelial dysfunction
Endothelial dysfunction is considered to occur early in patients with insulin resistance and to precede morphological alterations like arterial stiffening or atherosclerosis. Endothelial cells regulate the vascular tone by the release of vasoactive substances like nitric oxide or endothelin 1.In addition, endothelial cells modulate platelet function, inflammatory activity, vascular smooth muscle growth and migration.
Impairment of endothelial function seems to precede the development of diabetes as it was observed in subjects with impaired glucose control and first degree relatives without diabetes of patients with diabetes mellitus (1,2). Endothelial dysfunction can be measured by different methods using invasive or non-invasive technologies.
Coronary angiography with acetylcholine stimulated coronary blood flow is considered as a gold standard for the evaluation of endothelial function in coronary arteries (3). Due to the invasive procedure and the high costs, this technology it is not widely used.
Flow mediated dilatation (FMD) of the brachial artery has become the most used alternative for the assessment of endothelial function in large conduit arteries. This technology is based on a doppler ultrasound visualisation of the arterial diameter before and after the induction of local ischemia. The percent increase in arterial diameter after the release of a cuff placed at the forearm is calculated and considered to reflect the flow mediated release of nitric oxide from endothelial cells (4).
Several studies showed that FMD is a predictor of future target organ damage and cardiovascular events. As this technology is non-invasive and much less expensive, it is widely used for the assessment of endothelial function in clinical studies.
The reproducibility of FMD readings is highly dependent on operator expertise and requires a high standardisation of the procedure. Measurement of digital pulse amplitude tonometry (PAT) is based on the same principles as FMD. This technology uses a photoplethysmographic probe to record pulse wave amplitudes before and after reactive hyperaemia in the fingers. The reactive hyperaemia index (RHI) is calculated as the ratio of post deflation to baseline pulse amplitude in the hyperaemic finger in relation to the pulse amplitude in the contralateral finger (5). Both brachial FMD and RHI are independent predictors of cardiovascular events and all-cause mortality (6,7).
Atherosclerosis
Carotid intima-media thickness (C-IMT) is used as biomarker of subclinical atherosclerosis. Increased C-IMT and the presence of carotid plaques are considered as indices for atherogenesis. An increased C-IMT was shown to be associated with an increased risk for cardiovascular events and mortality (8-10). C-IMT is defined as the thickness of the tunica intima and tunica media in different segments of the extracranial carotid tree assessed with high-resolution ultrasound. While an isolated increase in C-IMT reflects early atherosclerotic changes, the additional presence of plaques stands for a more pronounced stage in atherosclerosis.
New advances like B-mode image processing based devices and radio-frequency-based echo-tracking systems can increase the precision and accuracy in the assessment of C-IMT. Moreover, high resolution magnetic resonance imaging (MRI) of the extracranial arteries can characterize the morphology of carotid plaques with regard to lipid content of the core, fibrous cap thickness, plaque bleeding and calcification; provide a more profound risk estimation for cardiovascular events. Patients with type 2 diabetes mellitus present with increased C-IMT, higher prevalence of plaques and higher plaque volume compared to healthy controls (11,12).
Arterial Stiffness
Arterial distensibility is used as a robust marker for structural and functional alterations in the arterial wall. Increasing arterial stiffness is caused by degenerative changes of extracellular matrix in the media layer which is distinct from the atherosclerotic processes taking place in the intima layer of the arterial wall.
Aging, hypertension, and diabetes mellitus affect the structural and functional properties of the vessels due to increased elastin fatigue fractures, collagen deposition and cross-linking. Multiple approaches to measure arterial stiffness are available and used in clinical studies.
The assessment of pulse wave velocity (PWV) is considered to reflect the elasticity of the arterial wall in between two different arterial segments. The pulse wave is recorded trans-cutaneously using mechano-transducers or applanation tonometers. In addition, pulse pressure waveforms can be recorded simultaneously with dedicated mechano-transducers attached to the skin, or sequentially from different sites with the calculation of transit times from a simultaneously recorded ECG.
PWV is calculated as the ratio of the distance to the time of the pulse wave within an arterial segment. Most commonly pulse pressure velocity is calculated from recordings at the carotid and the femoral artery. In patients with arterial hypertension or diabetes mellitus, an increase in PWV is associated with an increased risk of coronary artery disease, stroke, or peripheral artery disease (13-15).
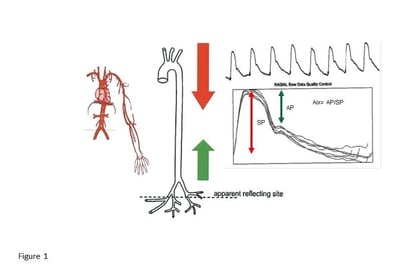
Figure 1: Assessment of Aix from peripheral arterial pulse wave form readings (Augmentation index (AU) = Augmentation pressure (AP) / Systolic pressure (SP); modified according to (18))
Morphological analysis of the pulse wave form provides a composite measure of arterial stiffness derived from central vascular distensibility and peripheral wave reflection due to the resistance of peripheral muscle arteries. The augmentation index (AIx) is used to characterize the elasticity of central arterial compartments. As shown in figure 1, the AIx is defined as the ratio between the second peak (central arterial elasticity and peripheral resistance) and the first peak (systolic blood pressure), obtained from averaged repeated pulse wave readings. As heart rate is an important covariant in the morphological analysis of pulse waves, Aix is usually corrected to a standard heart rate of 75 bpm (AIx@75). In a recent metaanalysis, Aix was shown to be an independent predictor for cardiovascular events and all-cause mortality in patients at cardiovascular risk (16). Different from PWV which measures the transmission of the pulse wave between in a defined arterial segment, the Aix is considered to represent the elastic properties of the overall arterial system (17).
References
- Caballero AE, Arora S, Saouaf R, Lim SC, Smakowski P, Park JY, King GL, LoGerfo FW, Horton ES, Veves A: Microvascular and macrovascular reactivity is reduced in subjects at risk for type 2 diabetes. Diabetes 48:1856-1862, 1999
- Vehkavaara S, Seppala-Lindroos A, Westerbacka J, Groop PH, Yki-Jarvinen H: In vivo endothelial dysfunction characterizes patients with impaired fasting glucose. Diabetes Care 22:2055-2060, 1999
- Ludmer PL, Selwyn AP, Shook TL, Wayne RR, Mudge GH, Alexander RW, Ganz P: Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med 315:1046-1051, 1986
- Green DJ, Dawson EA, Groenewoud HM, Jones H, Thijssen DH: Is flow-mediated dilation nitric oxide mediated?: A meta-analysis. Hypertension 63:376-382, 2014
- Rubinshtein R, Kuvin JT, Soffler M, Lennon RJ, Lavi S, Nelson RE, Pumper GM, Lerman LO, Lerman A: Assessment of endothelial function by non-invasive peripheral arterial tonometry predicts late cardiovascular adverse events. Eur Heart J 31:1142-1148, 2010
- Xu Y, Arora RC, Hiebert BM, Lerner B, Szwajcer A, McDonald K, Rigatto C, Komenda P, Sood MM, Tangri N: Non-invasive endothelial function testing and the risk of adverse outcomes: a systematic review and meta-analysis. Eur Heart J Cardiovasc Imaging 15:736-746, 2014
- Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, Lerman A: Prognostic Value of Flow-Mediated Vasodilation in Brachial Artery and Fingertip Artery for Cardiovascular Events: A Systematic Review and Meta-Analysis. J Am Heart Assoc 4: 2015
- Hodis HN, Mack WJ, LaBree L, Selzer RH, Liu CR, Liu CH, Azen SP: The role of carotid arterial intima-media thickness in predicting clinical coronary events. Ann Intern Med 128:262-269, 1998
- Chambless LE, Folsom AR, Clegg LX, Sharrett AR, Shahar E, Nieto FJ, Rosamond WD, Evans G: Carotid wall thickness is predictive of incident clinical stroke: the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol 151:478-487, 2000
- Rosvall M, Janzon L, Berglund G, Engstrom G, Hedblad B: Incident coronary events and case fatality in relation to common carotid intima-media thickness. J Intern Med 257:430-437, 2005
- Brohall G, Oden A, Fagerberg B: Carotid artery intima-media thickness in patients with Type 2 diabetes mellitus and impaired glucose tolerance: a systematic review. Diabet Med 23:609-616, 2006
- Pollex RL, Spence JD, House AA, Fenster A, Hanley AJ, Zinman B, Harris SB, Hegele RA: A comparison of ultrasound measurements to assess carotid atherosclerosis development in subjects with and without type 2 diabetes. Cardiovasc Ultrasound 3:15, 2005
- Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ: Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 121:505-511, 2010
- Wilkinson IB, Cockcroft JR, McEniery CM: Aortic stiffness as a cardiovascular risk predictor. BMJ 351:h3764, 2015
- Gasecki D, Rojek A, Kwarciany M, Kubach M, Boutouyrie P, Nyka W, Laurent S, Narkiewicz K: Aortic stiffness predicts functional outcome in patients after ischemic stroke. Stroke 43:543-544, 2012
- Vlachopoulos C, Aznaouridis K, Stefanadis C: Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 55:1318-1327, 2010
- Riggio S, Mandraffino G, Sardo MA, Iudicello R, Camarda N, Imbalzano E, Alibrandi A, Saitta C, Carerj S, Arrigo T, Saitta A: Pulse wave velocity and augmentation index, but not intima-media thickness, are early indicators of vascular damage in hypercholesterolemic children. Eur J Clin Invest 40:250-257, 2010
- Wilhelm B, Klein J, Friedrich Ch, Forst S, Pfützner A, Kann P, Weber M, Forst T.: Increased arterial augmentation and augmentation insdex as surrogate parameters for arteriosclerosis in subjects with diabetes mellitus and non-diabetic subjects with cardiovascular disease. J Diabetes Sci Technol 2:260-263, 2007