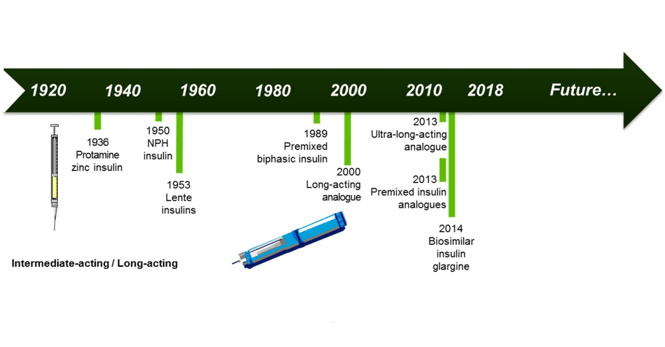
Long-acting insulins have been developed for patients with diabetes to provide a basal insulin cover during the day and night. The first slow-release formulations used protamine and/or zinc to achieve a duration of action up to 16 hours. Since 2000 insulin analogues with different mechanisms of protraction are available and achieve a predictable glucose lowering effect with one daily injection. Currently, ultra-long acting insulin analogues are available that have a duration of action beyond 24 hours. This prolonged duration of action reduces day-to-day variability and offers daily dosing flexibility [1]. What further improvements in basal insulin therapy can be expected in the future and what exactly does the ideal basal insulin look like?
Injection therapy
Most patients with diabetes who are using insulin therapy take a daily basal insulin injection, either as monotherapy, in combination with oral anti-diabetes agents or as part of a multiple daily injection (MDI) regimen. The next step in development for long-acting insulin injections would be to provide a duration of action far beyond 24 hours to avoid the need for daily injection. A basal insulin injection once every 2 days would already significantly reduce the amount of injections per patient. But having to give injections on different weekdays may not be an ideal treatment regimen. A regimen with once-per-week injection on a fixed day of the week would be much easier to implement and reduces the number of injections by a factor 6 compared to daily administration. A number of companies, including AntraBio, now Rezolute [2], Hanmi pharmaceuticals [3] and Novo Nordisk [4], have shared some information on their new once-weekly insulin formulations, but with limited clinical experience, questions on the feasibility and long-term safety of such a once-weekly regimen remain. In theory, the much longer half-life of these new formulations will produce a peakless insulin action profile during a dosing interval (1 week). With such a flat weekly profile, the variation in day-to-day insulin action can be expected to be minimal. Once-weekly insulins are therefore believed to provide a more reproducible and predictable glucose lowering effect than existing (ultra-) long-acting insulin analogues, which should facilitate titration to achieve better metabolic control without an increased risk of hypoglycemia.
Pump therapy
Insulin pump therapy can replace MDI therapy and is used by an increasing amount of patients with type 1 diabetes. Pump therapy is still rather uncommon for the treatment of type 2 diabetes [5], but more and more data [6] is being generated showing potential advantages of pump therapy for this patient population compared to injection therapy. Instead of injecting an insulin with a prolonged duration of action, basal coverage by insulin pump therapy is provided through the continuous infusion of a short- or rapid-acting insulin. Short- and rapid-acting insulins are used, not only so that the same pump can infuse bolus amounts of insulin to also allow prandial insulin coverage, but also so that the basal rate pattern can be varied during times of the day, including its complete interruption. As with injection of very long-acting insulin analogues, a flat insulin action profile can be achieved using pump therapy with a constant basal infusion rate, providing the same advantages as mentioned above: a reproducible and predictable glucose lowering effect. However, many patients choose to program different hourly basal rates to adapt to circadian changes in insulin sensitivity and for example increase insulin delivery overnight to counteract the dawn phenomenon. Whether a more variable basal rate pattern is advantageous in terms of metabolic outcomes is still a matter of debate [7]. However, a case for more variation in basal insulin administration can be made when one considers the data generated with closed-loop devices. The combination of insulin pump therapy with continuous glucose monitoring and automated basal rate adjustment has shown that individual basal insulin needs vary widely [8] from day-to-day and between different parts of the day. Especially during the night time, individual insulin requirements to achieve good glucose control varied between 50% on some nights to 300% on other nights compared to the subject’s usual insulin dose before starting the closed-loop therapy. This example shows that large variation in (basal) insulin administration (at the right time) may be needed to achieve low variation in blood glucose concentrations.
Other basal insulin developments
Therapeutic inertia [9] is pronounced for starting insulin therapy in type 2 diabetes and is commonly attributed to fear of injections and fear of hypoglycemia. An alternative route of administration of insulin, for example via oral administration in the form of an insulin tablet, would be obviously beneficial and more convenient for patients. Furthermore, oral insulin administration results in a more physiological insulin delivery [10], because the absorption via the portal vein mimics more closely pancreatic insulin secretion. In a recent article [11] in The Lancet that we published together with authors from Novo Nordisk, we investigated the efficacy and safety of an oral basal insulin versus injection of the long-acting insulin glargine. The main outcome of the trial was that the oral basal insulin could control fasting glucose levels in a safe manner to the same extent as the commercially available and widely used insulin glargine after 8 weeks of treatment. This is a great achievement and created a lot of enthusiasm [12] for the future development of oral insulin. Nevertheless, the development of this particular oral basal insulin was stopped due to relatively low absorption and subsequent need for administration of high insulin amounts (=high costs) to achieve a metabolic effect. Better technologies to increase the absorption of insulin in the gastro-intestinal tract are therefore needed and being explored [13].
The ideal basal insulin
The question that remains is, what is the ideal basal insulin? Is an adaptive, variable basal infusion rate with pump therapy better than the peakless profile of long-acting insulin injections? Perhaps. But not all patients want to carry or can simply afford a complete closed-loop system that needs to be worn for 24 hours per days, when they can achieve quite good control with an insulin shot that only needs to be given once per week. Another step towards an ideal basal insulin may be the development of a glucose-responsive or smart insulin [14]. A glucose-responsive insulin could be administered easily without the need for a pump system and in theory always provides the right amount of insulin to keep glucose levels fairly constant, i.e. these insulins mimic the glucose-responsive capabilities of a healthy pancreas. In practice, the glucose-responsiveness [15] of such a new insulin may not always be as good as expected, but with a diverse number of approaches in the pre-clinical pipeline, there is an expectation that the development of these insulins will accelerate soon.




