The liver‘s specific anatomical conditions and functions in systemic metabolism and defense provoke a hepato-centric view on the pathogenesis and treatment of diabetes. Whereas the contribution of the liver as a glucose supplier to the development of hyperglycemia and associated comorbid conditions is well recognised (DeFronzo, 2009) its involvement beyond the provision of too much glucose has been unravelled more recently (Stefan & Häring, 2013).
Part I of this „liver first ?“ blog focuses some less common aspects of the „glucostat“ function of the liver (Jungermann & Thurman, 1992), the hepato-peripheral insulin gradient (Matteucci et al., 2015), and the liver-pancreas axis (Turner & Holman, 1976; Ouaamari et al., 2016). We also discuss some conditions under which the liver needs specific consideration when designing clinical trials for the development of new drugs for the treatment of diabetes. In Part II we are going to adapt a more non-glucocentric viewpoint on systemic interactions of the liver in the evolution of type 2 diabetes and comorbid conditions.
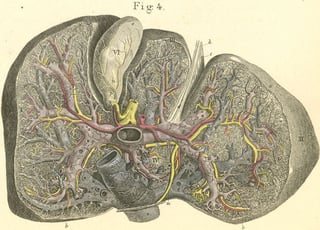 Figure: Atlas of Human Anatomy, 1841 in Leipzig Germany. 33-4 The division of blood vessels in the inner half of the liver, seen from its inferior surface.
Figure: Atlas of Human Anatomy, 1841 in Leipzig Germany. 33-4 The division of blood vessels in the inner half of the liver, seen from its inferior surface.
Context
Diabetes is a systemic disease precipitated by a heterogenous panel of risk factors and conditions. These include but are by far not limited to obesity and liver disease including a fatty degeneration of the liver. In our view pro-diabetic risk factors and conditions at the molecular level trigger the activity of vicious circles comprising, among others, glucose, cytokines, and reactive oxygen species. In the healthy state effective anti-hyperglycemic, anti-inflammatory, and anti-oxidative defense lines keep circle activities below a pathogenetically relevant threshold, safeguarding the physiological role of glucose, cytokines and reactive oxygen species in signal transduction, energy metabolism, and tissue functions. In the course of (pre)diabetes the autoamplificatory nature of the circles becomes prevailing due to an increased action of pro-diabetic risk factors and conditions and due to defects in counteracting defense mechanisms. In that case hyperglycemia, (pro)inflammatory states and oxidative stress may trigger progressively irreversible processes eventually accounting for beta-cell dysfunction and death, the development of insulin resistance, and other manifestations of diabetes and its comorbid conditions.
As the liver is a key player in orchestrating systemic energy metabolism as well as anti-inflammatory and antioxidative defense lines, a pivotal role in the pathogenesis of (pre)diabetes seems obvious.
A glucocentric view on the liver
Hepatic glucose sensing – the „portal signal“
There exists a hepatic „glucose paradox“: only low rates of glycogen synthesis despite the presence of both glucose and insulin were observed in isolated hepatocytes (Katz & McGarry, 1984), in humans receiving intravenous glucose infusion (DeFronzo et al., 1978), in rat livers perfused with equally concentrated glucose solutions through the portal vein and the hepatic artery (Gardemann et al., 1986), and in conscious dogs receiving glucose infusions via a peripheral vein under the condition of a pancreatic clamp (Cherrington, 1988). However, upon oral glucose ingestion the capability of insulin to stimulate hepatic glycogen synthesis is much higher. This is because orally ingested glucose enters the liver via the portal vein, thereby mounting a glucose concentration gradient between the portal vein and the hepatic artery (Stümpel & Jungermann, 1997). The portal-arterial glucose gradient creates the socalled the „portal signal“ which amplifies hepatic glucose uptake in the presence of insulin and rapidly increases glycogen deposition in the liver. The „portal signal“ can be mimicked by acetylcholine and may be sensed by intra-hepatic muscarinic nerves.
What’s the physiological meaning of the „portal signal“ ? The „portal signal“ enables the liver to differentiate between basal fluctuations of endogenous glucose (almost equal glucose concentration in both hepatic artery and portal vein, no need for a net hepatic glucose uptake) and glucose increases related to an oral glucose load (subject to hepatic glucose disposal): ony orally ingested glucose mounts the „portal signal“ and makes the liver permissive for a net glucose uptake. It has been suggested that the „portal signal“ may account for hepatic glucokinase activation thereby increasing glycogen synthesis in the liver (Cherrington, 1998). To which extend an impairment of portal signalling could contribute to the reduction of hepatic glucose uptake observed in patients with type 2 diabetes (Basu et al., 2000; Krssak et al., 2004) is currently not exactly known.
It is noteworthy that the „portal signal“ impacts the pharmacodynamic characterisation of oral insulin preparations. Its absence in case of an intravenous glucose administration should be considered when taking advantage of the hyperinsulinemic euglycemic glucose clamp technology (Heise et al. 2016). The time-action profiles based on intravenous glucose infusion rate – time curves by nature don’t capture the specific potential of oral insulins to increase hepatic glucose disposal. One option to address the impact of oral insulins on net hepatic glucose disposal in the setting of hyperinsulinemic euglycemic clamp investigations would be to artificially mount the „portal signal“, e.g. by either combining both intravenous and oral glucose administration (deFronzo et al., 1978) or by applying a low-dose infusion of fructose (Petersen et al., 2001).
Insulin clearance – mounting a hepato-peripheral insulin concentration gradient
The liver is the organ establishing the hepato-peripheral insulin gradient observed under physiological conditions. Endogenous insulin first floods the liver via the portal vein. During the liver passage insulin becomes proteolysed by 50 – 70% as catalysed by the insulin-degrading enzyme. Only the residual insulin reaches the peripheral targets including muscle and fat tissue. The hepato-peripheral insulin gradient is of key for the physiological action of insulin such as the establishment of proper glycemic control. A relative hypo-insulinisation of the liver (coupled to a relative hyper-insulinisation of peripheral tissues) is a limitation of current insulin therapy as a subcutaneous insulin administration does not fully establish the hepato-portal insulin gradient (Evans, 2015). This may comprise the „glucostat“ function of the liver by increasing net hepatic glucose production related to both fasting and meal ingestion (Matteucci et al., 2015).
Research on insulin preparations preferentially targeting the liver such as oral insulins including the hepatic-directed vesicle insulin (HDV-I; Geho et al., 2014) or pegylated insulin lispro for subcoutaneous administration (Caparrotta & Evans, 2014) has the ambition to develop insulin preparations which establish a hepato-peripheral insulin gradient also in the condition of exogenous insulin administration.
When using insulin clamps with intavenous insulin administration for the investigation of whole body glucose fluxes the absence of a hepato-peropheral insulin gardient requires consideration for a proper interpretation and extrapolation of data (Farmer et al., 2014).
Hepatic glucose production and fasting insulin – a feedback loop between hepatocytes and beta-cells ?
According to the concept behind the Homeostasis Modell Assessment (HOMA) there is a feedback loop between liver and pancreas for control of fasting insulin levels (Turner & Holman, 1976). Seen from this perspective, glucose as produced by the liver essentially accounts for basal insulin release by the beta-cells, which in turn suppresses hepatic glucose production. In case of reduced insulin secretion due to a beginning beta-cell dysfunction endogenous glucose production gets somewhat relieved from its suppression which again utilises a higher proportion of the still accessible insulin secretion capacity. The corresponding increase in fasting blood glucose levels has been considered as an attempt to normalize insulin supply by the beta-cells, thereby restoring insulin levels needed for „normal“ cell growth and tissue function. Fasting hyperglycemia due to an increase of glucose production by the liver can be seen as a response counterregulating insulin deficiency. This interpretation reflects an early non-glucocentric idea about a liver-pancreas axis: In this perspective the maintenance of „normal“ fasting blood glucose concentrations can be considered of secondary biological priority. However, the hepatic compensation for insulin deficiency increases the systemic susceptibility to a manifestation of overt type 2 diabetes by already slight downward shifts in insulin sensitivity (Matthews et al., 1985).
Lessens from the liver-specific insulin receptor knockout (LIRKO) mouse – the liver-pancreas axis revisited
In LIRKO mice the insulin-receptor-dependent insulin signalling is specifically absent in the liver parenchymal cells (Michael et al. 2000). This makes it an outstanding model for investigating the impact of an almost complete hepatic insulin resistance on the evolution of diabetes and comorbid conditions.
LIRKO mice display a severe resistance of hepatic glucose production to suppression by insulin which is accompanied by an increase of phosphoenol pyruvate carboxykinase (PEPCK) and glucose 6 phosphatase mRNA levels. On the other hand no overt type 2 diabetes can be observed in the LIRKO mice. This could be explained by a compensatory beta-cell hyperplasia and a decreased insulin clearence by the liver.
The situation is different in mice lacking both the hepatic insulin receptor and the beta-cell insulin receptor (bIRKO/LIRKO mice, Okada et al. 2007). bIRKO/LIRKO mice are not able to develop beta-cell hyperplasia compensating for hepatic insulin resistance. This leads to overt type 2 diabetes and premature death. Also mice lacking both systemic expression of the cell cycle protein cyclin D2 and the hepatic insulin receptor (Georgia et al. 2010) develop type 2 diabetes, again due to the absence of a beta-cell proliferation compensating for hepatic insulin resistance. A compensatory beta-cell proliferation is virtually absent in case the insulin receptor knockout is specifically introduced to muscle (Brüning et al., 1988), adipose tissue (Blüher et al., 2002), or brain (Brüning et al., 2000).
Recently it has been suggested that a humoral non-neuronal cell autonomous factor may induce beta-cell proliferation in the LIRKO mice: LIRKO hepatocyte-derived factors stimulate mouse and human bera-cell proliferation in ex vivo assays, independent of ambient glucose and insulin levels (El Ouaamari et al., 2013 & 2015). Whereas betatrophin is no longer considered as a candidate protein endogenously stimulating beta-cell proliferation (Cox et al. 2016) the protease inhibitor SerpinB1 is currently under discussion to be the liver-derived secretory protein regulating beta-cell proliferation (Ouaamari et al., 2016). These findings suggest a key role of the liver-pancreas axis in adapting beta-cell mass and function to insulin resistant states and deserve further scientific corroboration.
In view of the scientific and ethical barriers to stem cell-based regenerative therapies of diabetes there is a high demand for pharmacological approaches to maintaining pancreatic islet viability and adaptative potential in people with prediabetes and patients with type 1 diabetes (e.g. for intensification and extension of the honeymoon phase) and type 2 diabetes. Candidate proteins from the insulin resistant liver secretome and its targets localised at the beta-cell may provide excellent guidance for developing drugs protecting beta-cell mass and function.
Part II
Click to read the second part of this post series. Best, sign up for our regular blog notification to ensure you will not miss any future posts.
Also, read about Profil's capabilities in NASH/NAFLD studies. And if you are interested int he topic: then we have a online seminar on NASH.




